Headlines about virtual reality (VR) often focus on how its revolutionizing the world of gaming. The technology enables users to experience replications of real-life scenarios by integrating computer-generated graphics, sounds, and other sensory input. Although you know what you’re seeing is artificial, your mind and body react as if it were natural. Therefore, VR’s ability to “con” our brain means that it has broad applications beyond entertainment and gaming: it may become an invaluable resource in the battle against mental illness.
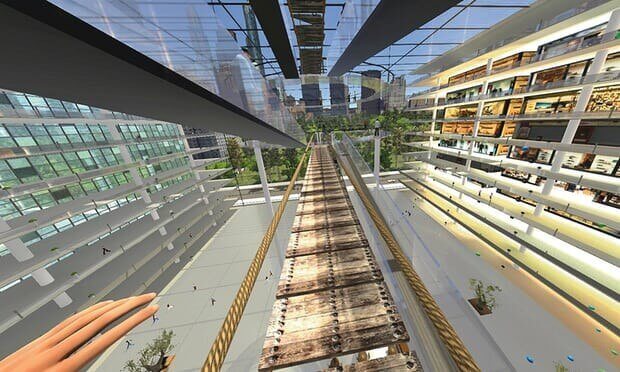
In fact, it already is. The most typical example is acrophobia (fear of heights). With VR exposure therapy (VRET), the person is helped to gradually face more challenging situations in three dimensions. These may involve a glass elevator ascending to higher floors of a virtual hotel. As the person is lifted up, the wind, the vibration, the stereotype sound of cars moving around are added to further create realism. The idea is to progressively teach the emotional part of the brain (the limbic system) that the object of your fear (height) is not associated with danger. What’s remarkable is that this VRET has led to significantly greater reductions in acrophobia symptoms compared with placebo or real exposure.
It isn’t just acrophobia that VR seems so well suited to tackling, the evidence is growing for its “magic” in treating other disorders including flying phobias, persecutory delusions, and — perhaps most well documented so far — Post Traumatic Stress Disorder (PTSD).

However, VR might not be a “magic pill” for all mental health issues. To date, there are only two small pilot studies examining the use of VR to combat depression, which of course is one of the most common psychiatric problems. Also, we know that the technology is effective to present individuals with simulations of the cues that lead to the cravings associated with alcohol abuse or excessive gambling, but no one has touched upon VR’s application in these areas. Similarly, VR may also allow anorexia patients to experience a healthy body so that they are less likely to overestimate their weight, but so far such studies for eating disorders still haven’t been considered methodologically sound.
We must remember that VR doesn’t merely enable us to simulate reality, it measures responses in circumstances where it might be costly (e.g., airplanes), impractical (eg., combat in Iraq) or ethically questionable (e.g., measuring sexual preferences) to be created in real life. VRET also affords full control over stimulus presentation, which is impossible for traditional experimental protocols. The therapist can set the intensity and specific aspects of the exposure environment according to each patient’s feared stimuli, thereby optimising individualised pacing. Indeed, it is not universally accepted that VR’s high level of sensory fidelity is always an advantage. Some researchers report physical and psychological side-effects induced by VRET. For instance, its greater degree of immersion would naturally imply an increase in dissociative experience (depersonalisation and derealisation) and lessen the user’s sense of presence in actual reality. VR is still far from perfect.





